Programs Offered
Associate in Applied Science Degree – Fall Admission
Associate in Applied Science Degree – LPN to ADN
Associate in Applied Science Degree – Spring Admission
Sample Courses
Practical Nursing & Associate Degree Nursing Program Philosophy
Mission
The Practical Nursing and Associate Degree program (hereinafter referred to as the nursing programs) support the mission of the North Carolina Community College System and the mission of Rowan-Cabarrus Community College. The faculty is committed to providing accessible high quality nursing education to meet the diverse and changing healthcare needs of the service area and to promoting the development of qualified graduates prepared for the professional role of Licensed Practical Nurse (LPN) and Registered Nurse (RN) at the entry level. Graduates of the nursing programs meet the education requirements to take the National Council Licensure Examination (NCLEX-PN)/ (NCLEX-RN).
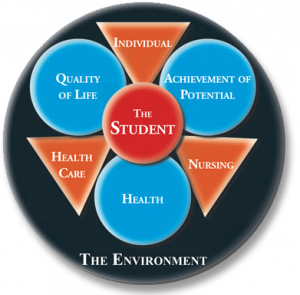
The philosophy of the nursing programs is derived from statements about the health, quality of life, achievement of potential, the individual, the environment, health, nursing practice, and education of both the practical and associate degree nurse. Within this mission, the goal of nursing faculty, through teaching excellence, is to promote the highest quality of nursing care to the individual, families and significant persons, and the community. Nursing faculty recognizes that the aim is to facilitate optimum health, quality of life and achievement of potential for the individual.
Nursing Education
Nursing education at the practical nursing level and the associate degree level in the North Carolina Community College System is a process that facilitates changes in behavior, the acquisition of knowledge, skills, and attitudes necessary to function as an entry level nurse. The curriculums are conceptually based and founded on the principles of adult and collaborative learning. Basic assumptions include self-direction, utilizing adult experiences, and problem- and activity-centered learning. The curriculums incorporate evidence-based nursing theory and practice, clinical judgment skills, general education, and the sciences in an environment conducive to learning. The conceptual design defines the essential elements as the environment, quality of life, achievement of potential, and health. The organizing framework contains content related to the individual, the health care system, and nursing.
The nursing programs at Rowan-Cabarrus Community College provide an education that is flexible, progressive, and sensitive to the changing needs of the individual, significant support person(s), and community. Through these educational experiences, students will have the opportunity to develop critical thinking and critical thinking skills. Learning is a continuous process that results in a change of behavior and occurs when the individual is challenged and motivated to enhance personal knowledge. Teaching and learning is an interactive collaborative process between teacher and learner. The responsibility of the faculty of Rowan-Cabarrus Community College Nursing Programs is to facilitate the student’s understanding and ability to meet the competencies for nursing practice through the design and evaluation of learning experiences. The nursing student is responsible for actively participating in learning experiences and the development of knowledge, skills, and attitudes necessary to provide quality individual centered nursing care.
The Practical Nurse – Dependent Role in Nursing
The graduate of the Practical Nursing program at Rowan-Cabarrus Community College is prepared to practice as an entry level nurse. The practice of the Licensed Practical Nurse, (LPN) is directed toward meeting the health care needs of individuals throughout their lifespan. Their role is supported by evidence-based clinical practice with the provision of care for individuals and families in structured settings. The LPN functions in a dependent role under the supervision of the registered nurse (RN) and other health care providers approved by North Carolina law. In accordance with the North Carolina Board of Nursing Administrative Code 21NCAC 36.0225 ‘Components of Nursing Practice for the Licensed Practical Nurse,’ the LPN accepts assignments that can be safely performed and participates in assessing, planning, implementing and evaluating the client’s response to health care interventions. The PN graduate demonstrates the competencies identified by the National League of Nursing (2010), the National Research Council (2003) and the Nursing Practice Act of North Carolina to provide nursing care. The practical nurse graduate is prepared to be a responsible life-long learner.
The Associate Degree Nurse – Independent Role in Nursing
The graduate of the Associate Degree nursing program at Rowan–Cabarrus Community College is prepared to meet the educational competencies defined by the National League for Nursing (2010), the National Research Council (2003) and the Nursing Practice Act of North Carolina. The practice of nursing is directed toward meeting the health care needs of individuals throughout their lifespan. The ADN prepared nurse’s role is characterized by evidence-based clinical practice with the provision of care for individuals and families in structured settings. The scope of RN practice is not defined by specific activities or tasks, but rather as a process, and is identified as independent and comprehensive. In accordance with the North Carolina Board of Nursing Administrative Code 21NCAC 36.0224 ‘Components of Nursing Practice for the Registered Nurse’, the RN safely accepts assignments that include assessing, planning and implementing nursing interventions and prescribed treatments for an individual, group, or community; as well as to evaluate responses to nursing care and treatment, and to collaborate with others as needed. The nursing graduate is prepared to be a responsible life-long learner.
Conceptual Framework
The conceptual model provides a framework to prepare learners for new instruction and motivates them by making a meaningful connection for the learner. The learner must attain mastery of each part of the framework; the individual, the healthcare system and nursing to understand the complete curriculum (Knowles, Holton, & Swanson, 2011). The domains of the individual, the healthcare system, and nursing provide the conceptual framework guiding the Practical Nursing and Associate Degree Nursing curriculums. Concepts are organized within each of these domains. Learning occurs from simple to complex.
Outcomes and competencies of the graduate are based on the NLN 2010 Outcomes and Competencies for Graduates of Practical Nursing and Associate Degree programs. The four outcomes/goals, Human Flourishing, Nursing Judgment, Professional Identity, and the Spirit of Inquiry are a part of the four conceptual framework domains of the curriculum. The domain of the Individual incorporates Human Flourishing. The domain of Nursing incorporates Nursing Judgment and Professional Identity. The Healthcare domain encompasses the Spirit of Inquiry. Competencies reflecting the IOM (2003) competencies: using informatics, employing evidence-based practice, providing client centered culturally competent care, managing client care, and participating in interdisciplinary teams, are integrated throughout the program. The NLN 2010 Core Values: caring, diversity, excellence, integrity, ethics, holism, and patient centeredness, are threaded throughout the curriculum.
Conceptual Framework Model – NCCCS ADN Programs
The Conceptual Model was adopted from the NCCCS for ADN programs but also is applicable to the Practical Nursing program with modification of scope of practice.
Conceptual Framework Model Definitions:
Achievement of Potential
Achievement of potential is the individual’s growth toward attaining one’s utmost ability and quality of life. It is based on the individual’s choices, perceptions, personal goals, life experiences, and holistic health.
Environment
The individual is in constant interaction with a changing environment that consists of both internal and external forces that varies throughout the lifespan and has the potential to cause stress in the individual. The nurse can assist the individual to alter aspects of the environment and to utilize his/her innate and learned coping mechanisms to adapt to these stressors.
Health
Health is a dynamic, ever-changing state of mental, physical, and spiritual well-being, which exists on a continuum from optimal wellness to illness and ending in death. The individual’s needs for healthcare are determined by his/her position on the continuum. Each individual’s health is based on his/her cultural perceptions and beliefs of health and illness and the ability to adapt to internal and external environmental forces. The individual is responsible for and capable of identifying, learning, and practicing health behaviors that can promote wellness, prevent illness, restore or maintain wellness, or achieve a dignified death.
Healthcare System
A system consists of the coming together of parts, the power comes from the energy of the interconnection and the way the parts come together. The community healthcare system is a macrosystem and consists of a variety of parts or microsystems. Clinics, hospitals, pharmacies, laboratories, long term care and Internet sites are microsystems that are connected by patients and information to improve health (National Research Council, 2003).
Individual
The faculty of Rowan-Cabarrus Community College believe that each individual is a complex, multidimensional, unique, and significant being possessing inherent value and worth, and a member of a family, community, and culturally diverse society. All individuals have dynamic bio-physical, psychological, socio-cultural, spiritual, and developmental needs that contribute to health, quality of life, and achievement of potential. Adaptation to the environment requires the individual to change throughout the lifespan. Each individual has a right to healthcare and to information that will assist him or her to participate actively in his or her health care in order to achieve the highest level of wellness possible. All individuals should be cared for, respected, nurtured, understood, and assisted. In order to provide care, nurses must view the individual at the center of any nursing activity.
Nursing
Nursing is a science and the art of integrating and assimilating knowledge and skills derived from biological, sociological, and behavioral sciences and information technology to deliver client-centered, culturally competent, holistic care. Through caring, empathy, ethics, and the development of a therapeutic relationship with the individual and significant support person(s), the nurse integrates the art of nursing with the scientific foundation for nursing practice that utilizes the nursing process. Incorporating documented best practice, while the LPN functions dependently, the RN functions independently and collaboratively with the interdisciplinary team to assist individuals to reach their maximum health potential through assurance of quality client outcomes, promotion of wellness, prevention of illness, and restoration of health or assistance in achieving a dignified death. Emphasis is also placed on cost-effective care to facilitate the achievement of positive individual and organizational outcomes.
Quality of Life
Quality of life involves five domains including physical, functional, psychological, social, and spiritual well-being. The individual’s perception of and satisfaction with activities of daily living contributes to their worth, meaning, or satisfaction. This empowers the individual to cope successfully with the full range of challenges encountered in the real world. (Ignatavicius & Workman, 2013).
Evaluative Framework – Tanner’s Clinical Judgment Model
The evaluative framework for the RCCC nursing programs provides a guide to promote the concept of clinical judgment. The framework recognizes that clinical judgment is a complex process that requires the nurse to understand the pathophysiological and diagnostic aspects of a patient’s clinical presentation as well as the physical, social, and emotional strengths of the patient and their family (Tanner, 2006).
The evaluative framework is based upon Tanner’s Clinical Judgment Model which includes four aspects: noticing, interpreting, responding, and reflecting. This model also connects to the National Council State Boards of Nursing Clinical Judgment Measurement Model, the Nursing Process, and the End-of-Program Student Learning Outcomes as shown in the chart below:
| Tanner’s Clinical Judgment Model | Clinical Judgment Measurement Model | Nursing Process | End-of-Program Student Learning Outcomes |
| Noticing | Recognize Cues | Assessment | Nursing Judgment |
| Interpreting | Analyze Cues | Analysis | Nursing Judgment |
| Interpreting | Prioritize Hypotheses | Analysis | Nursing Judgment |
| Interpreting | Generate Solutions | Planning | Nursing Judgment |
| Responding | Take Actions | Implementation | Human Flourishing and Nursing Judgment |
| Reflecting | Evaluate Outcomes | Evaluation | Professional Identity and Spirit of Inquiry |
These aspects are incorporated into the classroom, laboratory, and clinical settings to promote engaged moral reasoning, advanced clinical knowledge, and reflection-on-practice (Tanner, 2006).
End-of-Program Student Learning Outcomes – Practical Nursing
Graduates should be prepared to promote and enhance human flourishing for patients, families, communities, and themselves; to show sound nursing judgment; to continually develop their professional identity; and to maintain a spirit of inquiry as the move into the world of nursing practice, and beyond.
Upon completion of the Practical Nursing Program, the graduate will upon licensure…
- Human Flourishing: Promote the human dignity, integrity, self-determination, and personal growth of patients, oneself, and members of the health care team.
- Nursing Judgment: Provide a rationale for judgments used in the provision of safe, quality care and for decisions that promote the health of patients within a family context.
- Professional Identity: Assess how one’s personal strengths and values affect one’s identity as a nurse and one’s contributions as a member of the health care team (Professional Identity).
- Spirit of Injury: Question the basis for nursing actions, considering research, evidence, tradition, and patient preferences.
End-of-Program Student Learning Outcomes – Associate Degree Nursing
Upon completion of the Associate Degree Nursing Program, the graduate will upon licensure…
- Human Flourishing: Advocate for patients and families in ways that promote their self-determination, integrity, and ongoing growth as human beings.
- Nursing Judgment: Make judgments in practice, substantiated with evidence, that integrate nursing science in the provision of safe, quality care and promote the health of patients within a family and community context.
- Professional Identity: Implement one’s role as a nurse in ways that reflect integrity, responsibility, ethical practices, and an evolving identity as a nurse committed to evidence-based practice, caring, advocacy, and safe, quality care for diverse patients within a family and community context.
- Spirit of Inquiry: Examine the evidence that underlies clinical nursing practice to challenge the status quo, question underlying assumptions and offer new insights to improve the quality of care for patients, families, and communities.
NOTE: The 2010 NLN Educational Competencies for graduates of Practical Nursing and Associate Degree Nursing Programs have been adopted by the faculty as the Educational Outcomes for the RCCC nursing programs. The educational outcomes developed by the North Carolina Department of Community Colleges Curriculum Revision/Improvement Projects are incorporated into the Educational Outcomes of the PN and the ADN Nursing programs.
The Program Outcomes
The program outcomes of the Practical Nursing and Associate Degree Programs are the standards for measurement of the effectiveness of the curriculum design.
1. Performance on licensure exam
- The program’s most recent annual licensure examination pass rate will be at least 80% for all first-time test takers during the same 12-month period.
(NCBON standard – The Practical Nursing and Associate Degree Nursing programs shall maintain a three-year average at or above 95 percent of the national pass rate for licensure level pass rate on the first writing of the licensure examination).
2. Program Completion
- 60% of students entering the program for the first time will graduate.
3. Program satisfaction – Graduates will achieve the following outcome expectations:
- 90% express satisfaction with the program of learning
- 90% demonstrate satisfactory nursing practice to their employers reflecting the programs education outcomes.
4. Job Placement
- 90% of the students seeking employment will become employed as practical nurses or registered nurses within one year after graduation.
5. Lifelong learning (This outcome reflects the college’s mission and goals related to life-long learning)
- 80% of graduates will acknowledge the need for lifelong learning by participating in professional development activities.
6. North Carolina Board of Nursing Program Approval Status
- The Practical Nursing and Associate Degree Nursing programs will maintain full approval status.
7. Compliance with regulatory standards of the North Carolina Community College System and Southern Association of Colleges and Schools (SACS)
- The Practical Nursing and Associate Degree Nursing programs will be in compliance with the regulatory standards of these agencies.
8. Compliance with the regulatory standards of the Accreditation Commission for Education in Nursing (ACEN)
- The Practical Nursing and Associate Degree Nursing Programs will maintain compliance with the ACEN accreditation standards.
Glossary (PN and ADN Programs)
Caring: Caring is promoting health, healing, and hope in response to the human condition (NLN, 2007).
Client: any human being, regardless of sex or age. A person, family (or significant other), or community who enters the health care delivery system for assistance in meeting health needs. The recipient of care provided by health care providers including the practical nurse and the registered nurse. The term client denotes one who is a participant or collaborator in health care decisions affecting self or significant other(s).
Collaboration: Participation in an interdisciplinary health care team to promote safe, effective care and positive client outcomes.
Communication: Interactive process of exchange of information that may occur verbally, nonverbally, or through information technology.
Community: A group of people who reside in a specific locality, share government, and often have a common cultural, historical heritage, a social, religious, occupation, or other group sharing common interests or a common heritage, the public, or society.
Competency: A demonstrated cognitive, affective, and/or psychomotor capability derived from the activities of a nursing student in the various roles of the practice setting. Stated in broad performance terms, a competency is the integration of specific behaviors.
Concept: A concept is an organizing principle, or a classification of information (Giddens, 2013).
Core Competencies: The discrete and measurable skills, essential for the practice of nursing, that are developed by the faculty in schools of nursing to meet established program outcomes.
Core Values: Those beliefs or ideals which form the foundation for the work of a governing organization and/or nursing program.
Critical Thinking: Identifying, evaluating, and using evidence to guide decision making by means of logic and reasoning.
Culture: Comparative study and analysis of different cultures and subcultures in the world with respect to their caring behavior, nursing, care and health-illness values, beliefs, and patterns of behavior.
Differentiated Practice: The assignment of roles, functions, and work of nurses according to education, clinical reference, and defined competency and decision-making skills.
Distance Education: Distance education courses, allow students to participate in learning outside of the traditional classroom. Delivery methods are blended, internet, hybrid.
Blended: Primarily meets face-to-face on specified days and have a required online component, which requires students have Internet access as part of the course.
Internet: Internet students receive course instruction through the use of online content, email, and textbooks. Internet students complete their courses without on-campus meetings. Before beginning online courses, however, all Internet students are required to complete an online evaluation of their computer, email and Internet skills.
Hybrid courses combine online learning with face-to-face instruction. All Hybrid courses will meet on-campus on specified days. The remaining instruction and course content will be delivered as an Internet course.
*HyFlex (Hybrid Flexible) are courses in which 100% of the instruction is offered face-to-fect with the instructor in a physical classroom and 100% of the instruction is offered online allowing students an opportunity to choose whether to attend classes during regularly scheduled in-person sessions or participate online synchronously or asynchronously.
Diversity: Diversity means recognizing the differences among persons, ideas, values, and ethnicities while affirming the uniqueness of each (NLN, 2007).
Education: The process of imparting knowledge or skill through systematic instruction and the obtaining of knowledge or skill through such a process.
Ethics: Ethics in nursing integrates knowledge with human caring and compassion, while respecting the dignity, self-determination, and worth of all persons (NLN, 2007).
Evidence-based practice: Actions, processes, or methodologies that are grounded in and flow from the translation of substantive and current research. Integrate best research with clinical expertise and patient values for optimum care and participate in learning and research activities to the extent feasible (Finkleman, 2012).
Excellence: Commitment to continuous growth, improvement, and understanding (NLN, 2007).
Exemplar: Exemplars of a concept are specific examples that illustrate the broader concept and present alterations from the “normal.”
Holism: All living organisms are seen as interacting, unified wholes that are more than the sums of their parts (Berman and Snyder, 2012).
Human Flourishing: Encompasses the uniqueness, dignity, diversity, freedom, happiness, and holistic well-being of the individual within the larger family, community, and population (NLN, 2010).
HyFlex: Combines the terms “hybrid” and “flexible.” This refers to learning that integrates complimentary face-to-face and online learning experiences (both are synchronous at RCCC). Students can choose from one of two paths each didactic day: 1. Participate in face-to-face synchronous class sessions in the classroom, or 2. Participate in face-to-face synchronous sessions via video conference.
Informatics: Communicate, manage knowledge, mitigate error, and support decision making using information technology (Finkleman, 2012).
Institute of Medicine Competencies: The five core competencies identified by the IOM for healthcare providers are patient centered care, interdisciplinary teams, evidence-based practice, quality improvement, and informatics (National Research Council, 2003).
Integrity: Respecting the dignity and moral wholeness of every person without conditions or limitations (NLN, 2007).
Interdisciplinary Team: a group of health care providers from a variety of disciplines, who cooperate, collaborate, communicate and integrate client care and health promotion.
Interpreting: Generating hypotheses to support assessment data including patterns and cues. (Tanner, 2006)
Learning: is a continuous process that results in a change of behavior and occurs when the individual is challenged and motivated to enhance personal knowledge. Teaching and learning is an interactive process between teacher and learner. Learning is a lifelong process.
Life Span: the normal expected stages of growth and development from conception through advanced old age.
Managing Care: Integration of resources focusing on coordination of client care and supervision of nurses in the delivery of quality care.
Noticing: Understandings that collectively shape the nurse’s expectations for the patient (Tanner, 2006).
NLN Core Competencies: The eight core competencies outlined by the NLN are: professional behaviors, communication, assessment, clinical decision making, caring interventions, teaching and learning, collaboration, and managing care (NLN, 2000).
NLN Core Value: The core values as outlined by NLN are: caring, diversity, excellence, integrity, and ethics (NLN, 2010).
NLN Outcomes/Competencies: The outcomes/competencies for graduates of Practical Nursing and Associate degree programs include human flourishing, nursing judgment, professional identify and sprit of inquiry (NLN, 2010).
Nursing Judgment:
PN: Provide a rationale for judgments used in the provision of safe, quality care and for decisions that promote the health of patients within a family context (NLN, 2010).
ADN: Make judgments in practice, substantiated with evidence, that integrate nursing science in the provision of safe, quality care and promote the health of patients within a family and community context (NLN, 2010).
Nursing Process: A problem-solving approach to the identification of a client’s needs and the utilization of nursing interventions designed to promote adaptation in maintaining, restoring, and supporting health status. The major components of the process are assessment, analysis/diagnosis, planning, implementation, and evaluation.
Objectives: Specific, measurable behaviors. A hierarchy of objectives including educational objectives/outcomes, level objectives, course objectives, unit objectives, and specific learning objectives are used in the Rowan-Cabarrus Community College nursing programs as a guide for attaining desirable behaviors essential for the practice of nursing. The educational outcomes describe desirable behaviors in broad terms, while learning objectives are very specific.
Patient-centered: patient-centeredness is an orientation to care that incorporates and reflects the uniqueness of an individual patient’s background, personal preferences, culture, values, traditions, and family. Patient-centeredness supports the respectful, efficient, safe, and well-coordinated transition of the patient through all levels of care (NLN, 2010).
Patient Needs: Something essential for the physical and psychological well-being of humans. Categories of client needs are described as: safe, effective care environment, physiological integrity; psychosocial integrity, and health promotion/maintenance in accordance with the NCLEX-PN and RN Test Plan.
Professional Identity: Involves the internalization of core values and perspectives recognized as integral to the art and science of nursing (NLN, 2010).
Professional Identity –
PN: Assess how one’s personal strengths and values affect one’s personal identity as a nurse and one’s contributions as a member of the health care team (NLN, 2010).
ADN: Implement one’s role as a nurse in ways that reflect integrity, responsibility, ethical practices, and evolving identity as a nurse committed to evidence-based practice, caring, advocacy, and safe quality care for diverse patients within a family and community context (NLN, 2010).
Quality Improvement: Systematic processes to measure client outcomes, identify hazards and errors, and develop changes to improve client care.
Responding – Intervening in an intuitive and rational manner. (Tanner, 2006)
Reflecting – Connecting one’s actions to the outcomes that are generated. (Tanner, 2006)
Roles of the nurse: the function or practice of the practical nurse and registered nurse and encompasses the following:
- Provider of care involves the activities for direct hands-on care of the client
- Member within the discipline of nursing are behaviors which promote legal/ethical standards, accountable practice of nursing, and commitment to continued professional development for self and others.
- Manager of care, a role of the RN, involves activities of managing and delivering direct and indirect client care. Indirect care activities serve to enable caregivers to provide effective nursing care. Inherent in the three roles of the nurse are eight essential behaviors/competencies: professional behaviors, communication, assessment/nursing process, clinical decision-making, caring interventions, teaching and learning, collaboration, and managing care.
Scholarship: Activities that facilitate the enhancement of expertise and achievement of the goals and outcomes of the nursing education unit. This may include, but are not limited to: application of knowledge, teaching, service, practice, and research.
Significant Other: a person or group of people likely to have influence on and/or a close relationship with the client.
Society: the system or condition of living together as a community.
Spirit of Inquiry –
PN: Question the basis for nursing actions, considering research, evidence, tradition, and patient preferences
ADN: Examine the evidence that underlies clinical nursing practice to challenge the status quo, question underlying assumptions, and offer new insights to improve the quality of care for patients, families, and communities.
Structured Setting: an environment in which the policies, procedures, and protocols for provision of health care are established.
Teaching/Learning: Facilitator/facilitation of the acquisition of knowledge through learning.
Technology: a combination of equipment and software, used to meet educational outcomes, and to assist with instruction and learning experiences within the classroom.
Values: assumptions, convictions, or beliefs about the manner in which people should behave and the principles that should govern behavior.
References
Berman, A. & Snyder, S. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process and Practices (10th Ed.). Upper Saddle Creek, NJ: Prentice Hall.
Finkleman, A. (2012). Teaching IOM: Implications of the Institute of Medicine report for nursing education (3rd Ed.). Silver Spring, MD: American Nurses Association.
Giddens, J. (2013). Concepts for nursing practice. St. Louis: Elsevier Saunders.
Ignatavicius, D. & Workman, M. L. (2017). Medical-surgical nursing: Patient-centered collaborative care (9th Ed.). St. Louis, MO: Elsevier Saunders.
Institute of Medicine (2001). Crossing the quality chasm: A new health care system for the 21st century. Washington, D.C.: National Academy of Science. (Historical)
National League for Nursing (2018). NLN core competencies for Nurse Educators: A decade of influence. Washington, DC: NLN Publications.
National League for Nursing (2007). NLN core values. Washington, DC: NLN Publications. (Historical)
National League for Nursing (2012). Outcomes and competencies for graduates of practical/vocational, diploma, associate degree, baccalaureate, master’s, practice doctorate, and research doctorate programs in nursing. Washington, DC: NLN Publications.
National Research Council (2003). Health professions education: A bridge to quality. Washington, DC: The National Academies Press. (Historical)
Knowles, M., Holton, E., & Swanson, R. (2011). The adult learner. St. Louis: Elsevier Saunders.
Tanner, C. (2006). Thinking like a nurse: a research-based model of clinical judgment in nursing. Journal of Nursing Education, 45(6), 204-211.
Revised 06-19-2023